Prepare for breastfeeding and avoid common pitfalls that new mums face with Leila Ng Caceres, certified doula, birth and baby coach. She dishes out breastfeeding advice and techniques, so you can avoid the boobytraps and have a smooth-sailing nursing journey with your little one.
The Expert: Leila Ng Caceres
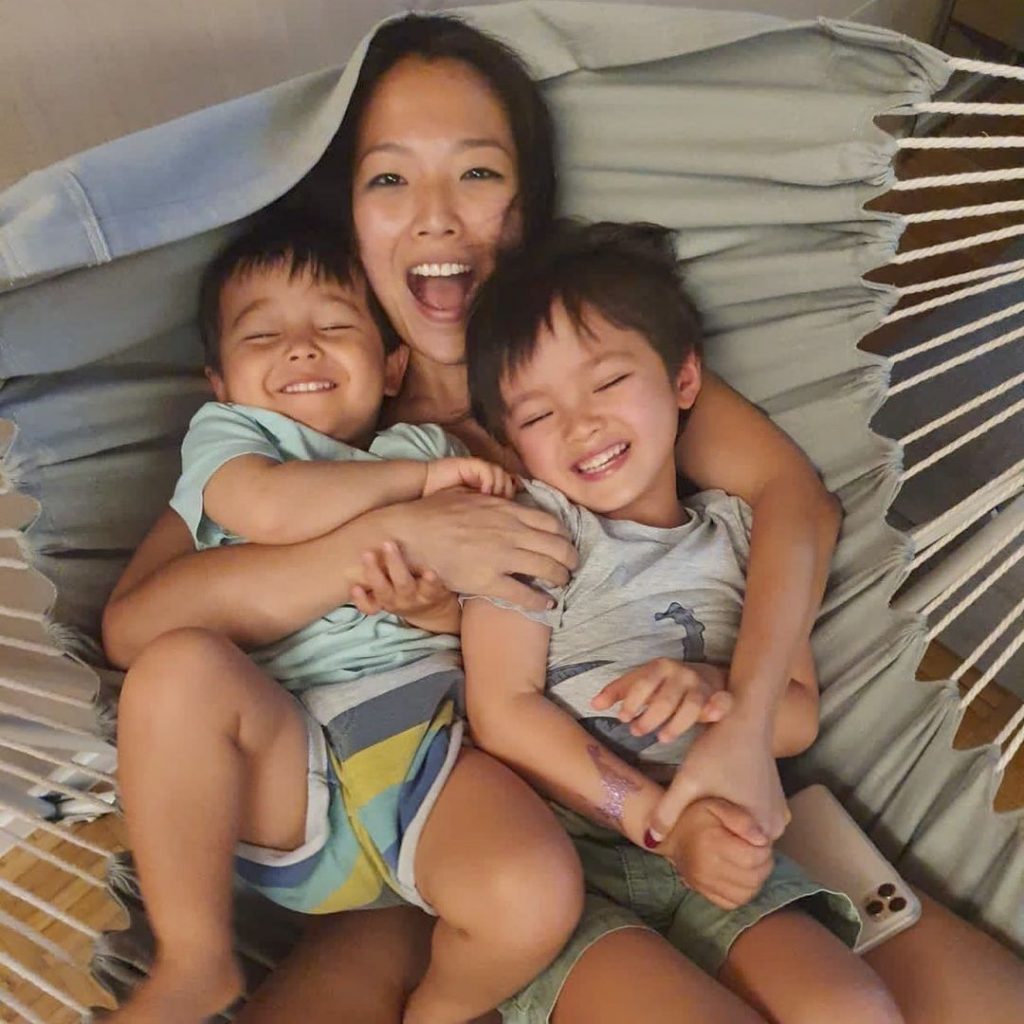
Leila Ng Caceres, is Singapore’s only US-trained and certified Lamaze Childbirth Educator and DONA Birth & Postpartum Doula. Founder of Leila & Co, Leila is currently pursuing her breastfeeding counsellor certification with Childbirth International. The mother of two also works closely with many top doctors and nurses from Singapore’s hospitals and helps women achieve the birth they desire.
Breastfeeding Advice for Expecting Mums

Leila advises first-time mums to “keep an open mind, get as much information as you can and allow yourself to experience breastfeeding – it will be your own unique experience.” For second or third-time mums, Leila says, “Scientific research has shown that with each subsequent pregnancy, breastfeeding gets easier!” Mammary tissues from the previous pregnancy remain, helping it respond quicker to subsequent pregnancy hormones. She explains, “Additional alveolar structures and epithelial cells are also created – leading to more and faster milk production.” Also, mothers are usually more experienced and less stressed than when they first breastfeed their newborns.
Establishing Your Supply
Prioritise taking care of yourself, eat healthily with meal services if necessary, and make sure to sufficiently hydrate yourself. Leila also suggests finding a comfortable spot for you to settle down to breastfeed. She says, “The more comfortable you are, the calmer you will be and that helps oxytocin (calm and love hormone) and prolactin (milk making hormone) to flow – thus making more milk!” Invest in a nursing armchair for good posture to ward off pesky aches and pains.
Next, watch your baby for early hunger cues, such as moving her fists to her mouth, sucking on her hands, or lip smacking. This makes it much easier to latch your baby on the breast. She may also want to feed more frequently than every two to three hours, so feed on demand rather than watching the clock. Mastering the side-lying position will also help you rest while your little one nurses – and naps too.
Safe Co-Sleeping
Your baby should always sleep in her cot, on a firm mattress with nothing else on the bed. However, co-sleeping helps mum and baby get more sleep. In such instances, ensure nothing obstructs your baby’s breathing and she doesn’t overheat. Also, make sure she sleeps on her back, and take care that she can’t fall out of bed or get trapped between the wall and the mattress. Avoid co-sleeping if you or your partner smoke, drink alcohol, or take drowsy medication. Refrain from sleeping on the aforementioned armchair as it can greatly increase the risk of SIDS. Try safe co-sleeping options such as the Hauck Face to Me and Chicco Next2me Forever Bedside Cots and Crescent Womb Infant Safety Bed ($99 to $690).
Must-Haves for Breastfeeding Success
Ensure you have a supportive breastfeeding team that includes your paediatrician, family, and friends. Don’t hesitate to call on your International Board certified lactation consultants, whenever you have doubts or questions. Other essentials include lanolin nipple creams and breastfeeding-friendly bras like the Bravado Nursing Bras ($49.90 to $79.90), and a supportive breastfeeding pillow ($29 to $135.90).
Breastfeeding Queries for New Mums

Getting Enough Milk
Leila says, “For newborns, since we can’t measure the input, we measure the output. If babies are hitting their wet and dirty diapers each day, and are gaining about 140-200g/week, you don’t have to worry!” As a gauge, your little one should have one dirty and wet diaper each for each day of life. For instance, on day 3, your baby should have three dirty and wet diapers each. After day 5, your little one should have at least three to four stools daily. Your baby’s diapers should weigh about the same as a wet diaper with three tablespoons of water. After this, she should have about five to six wet diapers every 24 hours.
Lip and Tongue Ties
Before you leave the hospital, do get the lactation consultant or the paediatrician to check your little one for a lip or tongue tie. Other indications may be painful breastfeeding even after a professional has checked your latch, damaged nipples or clicking sounds that do not go away.
Emptying Your Breasts
To promote your supply, you’ll need to keep removing milk so your breasts can make more. Leila says, “Fun fact! Your breasts are never truly empty at any time! Milk making is continuous and it is a supply-demand process.” Before latching, your breasts may feel firm and full, and softer once your baby has nursed.
Getting the Correct Latch
Leila says, “Breastfeeding is a learned skill, it might take a few tries to get the latch right.” The correct latch should be comfortable, with no pain, or slight pain when you initially latch your baby. Her lips should be flanged open, while her nose should not be blocked. Lastly, the dark circle around your nipple or your areola should be mostly inside your baby’s mouth.
Reducing Engorgement
Leila assures mums that “the initial engorgement of the breasts is normal for all mothers. It is a hormonal process. Your body converts all the milk-making (prolactin) hormones that have accumulated during pregnancy into milk, after the placenta has birthed, in one go.” Reduce engorgement by nursing your baby as much as possible, and reduce or avoid pumping. She explains, “Pumping actually signals to your breasts to make more milk as you are removing milk.”
Oversupply
Leila says, “There are a few important factors that contribute to the success of partial or full re-lactation. It is dependent on the age of the baby, the length of stopping and the willingness of the baby to go to the breast.” She adds that it may take a few weeks to a few months to see some results. Bring your baby to the breast frequently, empty the breast as much as possible, and pump after every feed. She says that some experts also recommend feeding baby supplemental milk through a supplemental nursing system that helps stimulate the breasts while your baby nurses.
If you’re keen to relactate, visit a lactation consultant – she can also advise if you need medication. In fact, Leila says, any time mums have “any doubts, fears, worries, concerns, problems or pain in any form around breastfeeding, they should see a lactation consultant.” Examples include pain during breastfeeding, nipple damage or if you feel your baby is not feeding well or growing.
Pumping Sessions While Caring for Babies on Your Own

Pumping with Electric Pump
If you’re breastfeeding well, and your baby is healthy and gaining weight, Leila says, “Most experts suggest holding off using the pump until your baby is four to six weeks old.” Thereafter, try pumping once a day for one bottle feeding, so your spouse or other caregivers can help feed your baby.
Pumping Sessions
Leila suggests getting between four to six sets of pump flanges and bottles. In a small basin of soapy water, soak your pump parts, bottles, and bottle nipples after each pumping and feeding session. Get your partner or parents or in-laws to help with the washing or feeding the baby. She adds, “I would also invest in a decent sized UV steriliser ($499 to $699).” Using this setup, you’ll properly wash and sterilise the bottles and nipples once or twice a day.
Caring for Babies While Pumping
Multitask pumping with feeding or getting your baby to sleep. Wear a hands free bra ($39.90) and hook yourself up to the pump. Prepare a bottle of milk and then feed your baby on your lap or a nursing pillow. Otherwise, try holding her in the space between your bottles like this video shows, to help put your baby back to sleep. Alternatively, put her in your lap, jiggling your leg or rocking her a little. You can also try a bouncer ($169 to $599) to rock her to sleep. For shorter pumping sessions, you can play with your little one as she tries out tummy time.
For an older baby, pump during her nap, or put her in a high chair ($299 to $504) and let her snack, or let her play with her toys. Other options include an activity centre ($99 to $249), going for a drive, or using handsfree pumps like the Elvie (up to $799).
Relactating
Leila says, “There are a few important factors that contribute to the success of partial or full re-lactation. It is dependent on the age of the baby, the length of stopping and the willingness of the baby to go to the breast.” She adds that it may take a few weeks to a few months to see some results. Bring your baby to the breast frequently, empty the breast as much as possible, and pump after every feed. She says that some experts also recommend feeding baby supplemental milk through a supplemental nursing system that helps stimulate the breasts while your baby nurses.
If you’re keen to relactate, visit a lactation consultant – she can also advise if you need medication. In fact, Leila says, any time mums have “any doubts, fears, worries, concerns, problems or pain in any form around breastfeeding, they should see a lactation consultant.” Examples include pain during breastfeeding, nipple damage or if you feel your baby is not feeding well or growing.
Breastfeeding Advice for Mums with Dysphoric Milk Ejection Reflex
If you feel ill, depressed or have extreme negative reactions when breastfeeding, you might have dysphoric milk ejection reflex. This is caused by an abrupt drop of dopamine, the brain hormone and neurotransmitter boosting and stabilising your mood. After your prolactin levels increase, your dopamine levels should also elevate. Leila shares, “Breastfeeding might not be for everyone. There are a lot of factors at play, hormones, pregnancy or birth trauma, maybe sexual trauma and PTSD and other mental health issues that can all contribute to extreme negative reactions when it comes to breastfeeding.” In such situations, Leila says, “If mothers feel severe negative emotions towards breastfeeding, we usually start by chatting with the mothers to find out what the issue(s) might be. Thereafter we might suggest they see either an IBCLC or a psychologist/psychiatrist, situation dependent.”
If mums decide to stop or not breastfeed, Leila says, “We will encourage the mother to do all research, learning and understanding all the risks and benefits… to make an informed decision.” She adds that “we will always support the mother to do what makes her feel empowered, confident and safe.”
Relevant Reads: Breastfeeding



